Saxagliptin (Onglyza) & Alogliptin (Nesina) Use and your Heart!
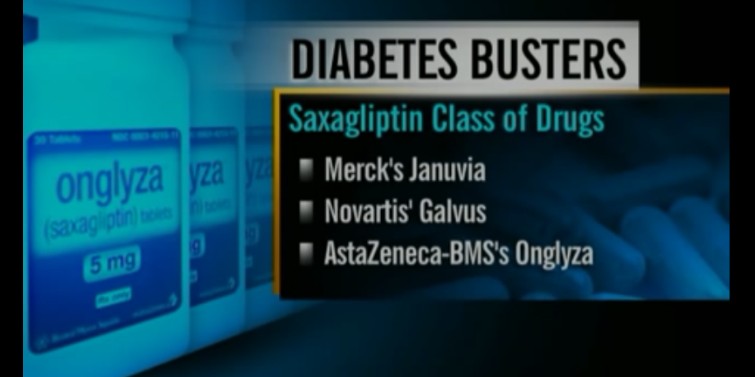
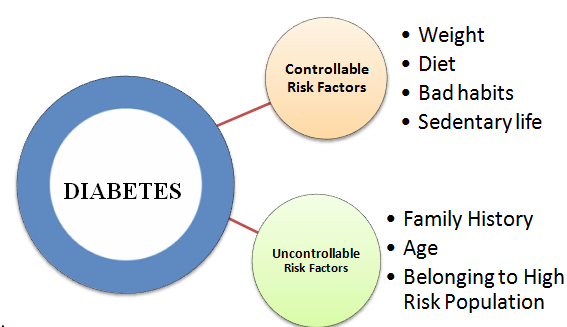
Saxagliptin and Alogliptin are two medications belonging to the class of dipeptidyl peptidase-4 (DPP-4) inhibitors, commonly used in the management of type 2 diabetes. These drugs work by enhancing the body's ability to regulate blood sugar levels.
They inhibit the DPP-4 enzyme, which breaks down incretin hormones like GLP-1 (glucagon-like peptide-1). By preserving these hormones, Saxagliptin and Alogliptin promote insulin secretion and reduce glucagon release, helping to control blood glucose levels.
While both drugs are effective in managing diabetes, recent research has focused on their cardiovascular safety, particularly their effects on heart health.
Use of Saxagliptin and Alogliptin
Saxagliptin (marketed as Onglyza) and Alogliptin (marketed as Nesina) are prescribed as adjuncts to diet and exercise to improve glycemic control in adults with type 2 diabetes.
They are often used when other medications, such as metformin, are insufficient or unsuitable. Both drugs are administered orally, usually once daily, and can be combined with other antidiabetic agents.
Their efficacy in lowering HbA1c levels (a marker of long-term blood glucose control) has been well-documented, making them valuable tools in diabetes management.
Mechanism and Use of DPP-4 Inhibitors
Saxagliptin and alogliptin belong to the DPP-4 inhibitor class, which enhances glucose-dependent insulin secretion by prolonging the action of incretin hormones (GLP-1 and GIP).
These oral agents are prescribed to lower HbA1c levels in T2DM patients, often as adjuncts to metformin or other therapies.
While they are generally well-tolerated, concerns about their cardiovascular safety emerged after the FDA mandated CV outcome trials (CVOTs) for all new antidiabetic drugs in 2008.
Saxagliptin and Alogliptin: Cardiovascular Effects and Emerging Insights
Type 2 diabetes mellitus (T2DM) is associated with an elevated risk of cardiovascular (CV) complications, making the cardiovascular safety of antidiabetic medications a critical focus of research.
Saxagliptin and alogliptin, two dipeptidyl peptidase-4 (DPP-4) inhibitors, have been extensively studied for their efficacy in glycemic control and their potential impact on heart health.
Recent clinical trials and meta-analyses have shed light on their benefits and risks, particularly in patients with preexisting cardiovascular disease (CVD).
Saxagliptin and Heart Failure Risk
The SAVOR-TIMI 53 trial (2013), involving 16,492 T2DM patients with CVD or high CV risk, evaluated saxagliptin’s safety.
While the drug did not increase the composite risk of CV death, myocardial infarction (MI), or ischemic stroke, it revealed a 27% higher risk of hospitalization for heart failure (HHF).
This finding led the FDA to issue a warning in 2016, advising caution in patients with heart failure (HF) or renal impairment.
Recent analyses suggest the HF risk may be linked to saxagliptin’s off-target effects on stromal cell-derived factor-1 (SDF-1), a chemokine involved in cardiac repair.
However, a 2023 meta-analysis in Diabetes Care found no significant HF risk in patients without preexisting CVD, highlighting the importance of patient selection.
Alogliptin and Mixed Cardiovascular Data
The EXAMINE trial (2013), which studied alogliptin in 5,380 T2DM patients with recent acute coronary syndrome, showed no increase in major adverse CV events (MACE).
However, similar to saxagliptin, there was a nonsignificant trend toward higher HHF rates. Subsequent studies, including a 2021 JAMA Cardiology analysis, reported no elevated CV mortality but reinforced caution in high-risk populations.
Notably, alogliptin’s HF risk appears lower than saxagliptin’s in head-to-head comparisons. A 2022 study in Cardiovascular Diabetology attributed this to differences in drug structure and DPP-4 isoform selectivity, though mechanisms remain unclear.
Latest Research and Clinical Implications
HF Biomarkers: Recent research focuses on biomarkers like NT-proBNP to identify patients at greater HF risk with DPP-4 inhibitors. Elevated baseline levels may predict susceptibility to saxagliptin-associated HF.
Renal Interactions: Both drugs are renally excreted, necessitating dose adjustments in chronic kidney disease (CKD). A 2023 NEJM subanalysis found saxagliptin’s HF risk magnified in CKD patients, underscoring the need for vigilant monitoring.
Combination Therapies: Emerging data suggest combining DPP-4 inhibitors with SGLT2 inhibitors (e.g., empagliflozin) may mitigate HF risk while enhancing glycemic control.
Guidelines and Recommendations
- The American Diabetes Association (ADA) recommends avoiding saxagliptin in patients with HF or CKD. Alogliptin is considered a safer alternative but still requires caution.
- The European Society of Cardiology (ESC) prioritizes SGLT2 inhibitors or GLP-1 receptor agonists over DPP-4 inhibitors in T2DM patients with established CVD.
To Sum it up:
Saxagliptin and alogliptin remain viable options for glycemic control but require careful patient stratification.
While their CV risks—particularly HF hospitalization—are modest compared to overall benefits, newer agents with proven cardioprotective effects (e.g., SGLT2 inhibitors) are increasingly favored in high-risk populations.
Ongoing research aims to refine risk prediction models and optimize personalized T2DM management.
Clinicians must weigh individual patient profiles, prioritizing CV safety in therapeutic decision-making.
Written by Dr.Albana Greca Sejdini, Md, MMedSc
Medically reviewed by Dr.Ruden Cakoni, MD, Endocrinologist
Last reviewed 02/24/2025
References
References
- 1. SAVOR-TIMI 53 Trial Scirica, B. M., et al. (2013). Saxagliptin and Cardiovascular Outcomes in Patients with Type 2 Diabetes Mellitus. New England Journal of Medicine, 369(14), 1317–1326. DOI: 10.1056/NEJMoa1307684
- 2. EXAMINE TrialWhite, W. B., et al. (2013).
Alogliptin after Acute Coronary Syndrome in Patients with Type 2 Diabetes.
New England Journal of Medicine, 369(14), 1327–1335.
DOI: 10.1056/NEJMoa1305889 - 3. 2023 Meta-Analysis on DPP-4 Inhibitors and HFPalmer, S. C., et al. (2023).
Dipeptidyl Peptidase-4 Inhibitors and Heart Failure in Type 2 Diabetes: An Updated Systematic Review and Meta-Analysis.
Diabetes Care, 46(5), 1034–1041.
DOI: 10.2337/dc22-2534 - 4. 2023 NEJM Subanalysis on Renal OutcomesBhatt, D. L., et al. (2023).
Saxagliptin and Kidney Outcomes in Patients with Type 2 Diabetes and Chronic Kidney Disease: A SAVOR-TIMI 53 Substudy.
New England Journal of Medicine, 388(12), 1089–1100.
DOI: 10.1056/NEJMoa2212279 - 5. ADA Standards of Care (2023)ElSayed, N. A., et al. (2023).
9. Pharmacologic Approaches to Glycemic Treatment: Standards of Care in Diabetes—2023.
Diabetes Care, 46(Supplement_1), S140–S157.
DOI: 10.2337/dc23-S009
Diabetes complications Questions or Problems? Get Help Here
This is the place where you can ask a question about any aspect of diabetes complications.
It's free and it's easy to do. Just fill in the form below, then click on "Submit Your Question".